Competing Mechanisms Influence Tumor Cell Migration

Color map showing the distribution of pressure across the gel region (between the two rows of semi-circular posts) containing the cancer cells.
It’s no secret that cancer is deadly. But did you know that it’s actually the uncontrolled spread of cancer throughout the body that most often leads to death? Understanding how cancer cells break loose from their original tumor, make their way into the body’s vascular system, and travel to another location is a critical step in the fight against cancer.
Roger Kamm, Singapore Research Professor of Biological and Mechanical Engineering at MIT, and Mechanical Engineering graduate student William Polacheck, in collaboration with Joseph Charest from the Charles Stark Draper Laboratory, have discovered that the direction in which fluid flows through bodily tissue determines how likely the cancer cells are to spread, or metastasize. Armed with that information, they say it may be possible to limit the spread of cancer.
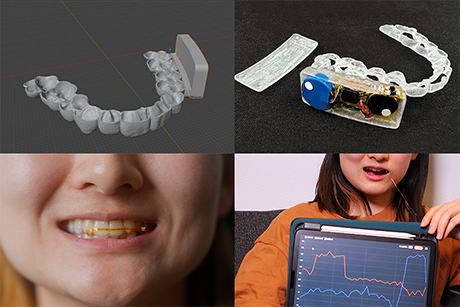
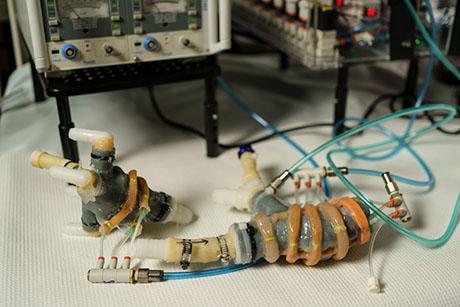
Almost as important as their discovery – published in Proceedings of the National Academy of Sciences – is the 3D microfluidic system they invented that allowed them to make it. Whereas previous insights were based solely on the visualization of individual cells in an artificial flow, Polacheck and Kamm’s system allows them to look at the way cells interact with tissue that mimics natural breast tissue.

Schematic showing the full microfluidic system used to generate interstitial flow for the study of cancer cell migration.
“There isn’t a single drug currently on the market that addresses how cancer cells break lose from a primary tumor and get into the vascular system, migrate out, and form a secondary tumor. But those are processes that we can actually simulate in our microfluidic system,” says Kamm.
It was the limitation of previous studies that fueled Polacheck, Charest, and Kamm to develop this system and investigate the migration of cancer cells, with the hope of discovering additional details that were previously undetectable.
The basis of their experiments was the underlying knowledge that, due to their continual growth, tumors generate high fluid pressure in surrounding tissues. This pressure, in turn, is known to generate a fluid flow away from the tumor. A former post doctoral student of Kamm’s, Melody Schwart (now a professor at École Polytechnique Fédérale de Lausanne) had previously discovered that, due to this flow, ligands secreted by a tumor cell selectively bind to receptors on the downstream side of the cell. She found that this process ultimately results in an asymmetry that stimulates cells to migrate in the direction of the flow.
If this were the full story, it would be a discouraging result, because it would mean that when the cells start to break lose from a tumor, they will automatically move toward the vascular system, thus spreading the cancer.
Luckily, the story continues. With their new 3D microfluidic platform, which consists of two channels separated by a region of single cells in a gel, or matrix, across which a flow can be generated, Polacheck and Kamm started experiments on breast cancer cells to simulate how the process of migration actually works in the context of the body—and hopefully build on Schwartz’s findings.
To their surprise, they found just the opposite: Instead of moving with the flow, as Schwartz had found, the cancer cells moved upstream. At first, they questioned their findings, but then Polacheck and Kamm realized that the cause of the discrepancy is the existence of two competing mechanisms.
One is autologous chemotaxis, which occurs in low-cell-density situations or when the CCR7 receptor becomes activated. Autologous chemotaxis increases the appearance of ligands at the downstream side of the cell, producing downstream migration, as Schwartz had found.
The other, they discovered, happens in high-cell-density situations – like around a growing tumor – or when the CCR7 receptor is blocked. This newly discovered mechanism kicks in when the pressure of a fluid flowing past a cell leads to the activation of a class of receptors called integrins, ultimately prompting upstream migration. Both mechanisms are due to asymmetry in a tumor cell’s interactions with its environment.
Polacheck and Kamm’s discovery could stop cancer dead in its tracks. “Acting on this might significantly improve cancer survival rates,” says Kamm. “Pharmaceutical companies can use this information to focus on creating drugs that would block the CCR7 receptor to prevent migration toward the vascular system, and confine the tumors.”
And it doesn’t end there. Because of its ability to mimic the interactions cells experience inside the body— using real human cells, in real time—Polacheck and Kamm’s system could be useful in a myriad of other biological studies as well, such as those focused on inflammation, liver disease, and liver toxicity, among others. “We’re finding that the ability to visualize the interactions between different cell types is critical to learning how the cells behave,” says Kamm.![]()